HMPV: A Rising Respiratory Threat Among Chinese Children
Introduction
Human metapneumovirus (HMPV) is a common respiratory virus that affects children worldwide. In China, HMPV has emerged as a significant public health concern, with increasing hospitalization rates and severe complications. This news article critically examines the complexities of HMPV infection in Chinese children, exploring its epidemiology, clinical manifestations, risk factors, and prevention strategies.
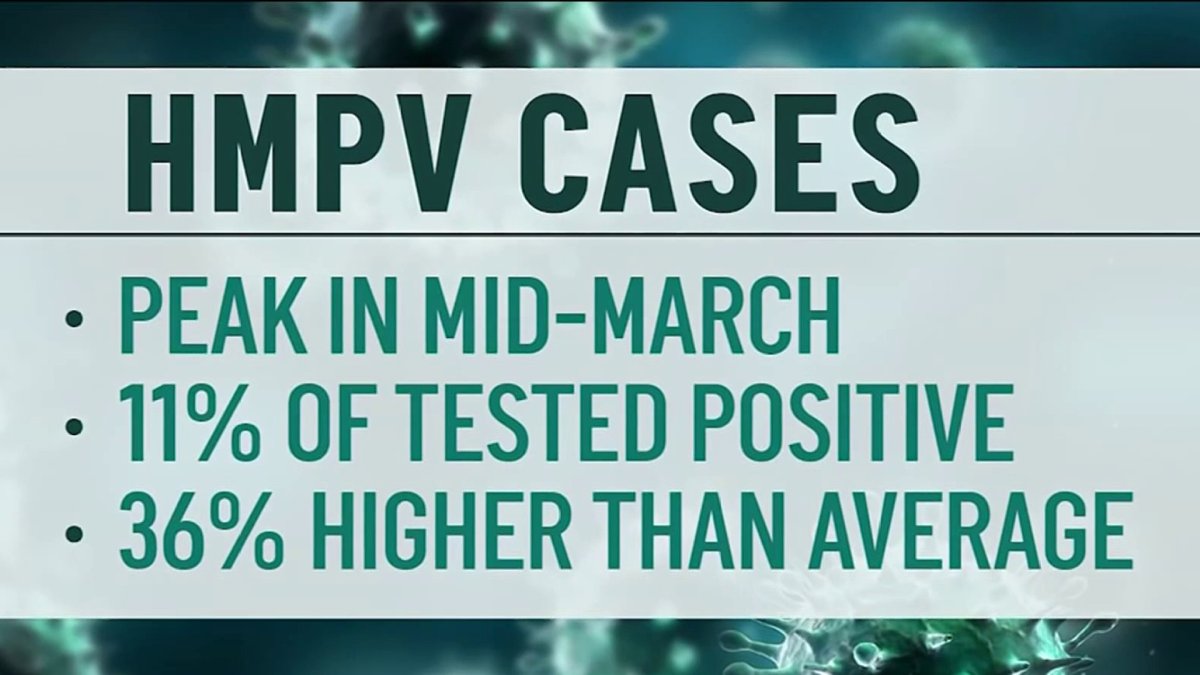
Epidemiology
HMPV is a seasonal virus, with a peak incidence during the winter months. In China, HMPV activity has been increasing over the past decade, becoming the second leading cause of viral lower respiratory tract infection (LRTI) among hospitalized children. Studies have shown that HMPV infections are more common in young children, especially those under the age of two, and premature infants.
The transmission of HMPV occurs through respiratory droplets and direct contact with infected individuals. Contact with contaminated surfaces can also play a role in transmission. Children in daycare settings, crowded households, and those with siblings attending school are at a higher risk of HMPV infection.
Clinical Manifestations
HMPV infection can present with a wide range of symptoms, from mild upper respiratory tract symptoms (URTI) to severe LRTI. Common symptoms include fever, cough, wheezing, and difficulty breathing. In severe cases, HMPV can lead to pneumonia, bronchiolitis, and hospitalization.
Young children are particularly vulnerable to severe HMPV infection due to their immature immune systems and smaller airways. Premature infants and children with underlying health conditions, such as heart or lung disease, are also at an increased risk of complications.
Risk Factors
Several risk factors have been identified for severe HMPV infection in Chinese children. These include:
- Age: Children under the age of two are at the highest risk.
- Prematurity: Premature infants are more likely to develop severe HMPV infection.
- Underlying health conditions: Children with heart or lung disease, immune deficiencies, or chronic respiratory conditions are at increased risk.
- Exposure to daycare or school: Children in daycare settings or those with siblings attending school are more likely to be exposed to HMPV.
- Crowded households: Children living in crowded households are at an increased risk of HMPV infection.
Prevention and Control
There is currently no specific antiviral treatment for HMPV infection. Preventive measures, such as vaccination, hand hygiene, and respiratory droplet precautions, are crucial in reducing the spread and severity of HMPV infection.
Vaccination: A vaccine against HMPV is currently in development. However, it is not yet widely available in China.
Hand hygiene: Frequent handwashing with soap and water or the use of alcohol-based hand sanitizers can help prevent the spread of HMPV.
Respiratory droplet precautions: Covering the mouth and nose when coughing or sneezing, and avoiding close contact with infected individuals, can help reduce transmission.
Conclusion
HMPV is a significant respiratory threat among Chinese children, particularly young children, premature infants, and those with underlying health conditions. Understanding the epidemiology, clinical manifestations, risk factors, and preventive measures of HMPV infection is crucial for healthcare professionals and public health officials in developing effective control and prevention strategies. Continued research and surveillance are needed to further elucidate the burden and impact of HMPV infection in China and to inform evidence-based public health policies.

Post a Comment